by NAMAS
Mar 20th, 2020
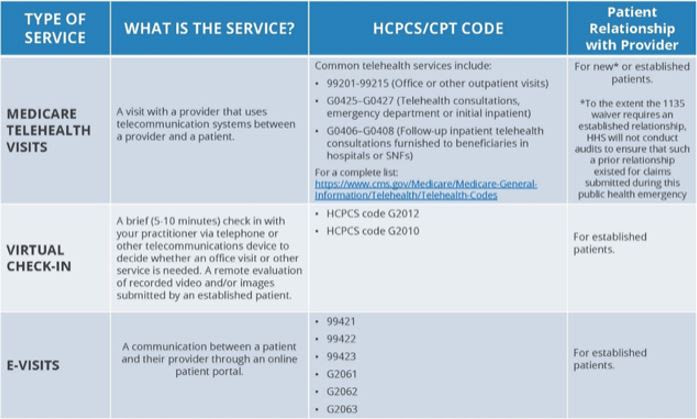
The following is a step-by-step guide on how to convert office-based encounters to telehealth encounters during the current COVID-19 pandemic. These rules may change post-pandemic, as many changes relaxing existing rules were made on a temporary basis by CMS and commercial payers to facilitate patient access and minimize risk of infection.
- Patient name and date of birth
- Date of service
- Rendering provider
- Elect services as a telehealth encounter
- Instructions regarding the proper location for the patient during the telehealth encounter
- Patient vs. provider responsibilities in case of technical difficulties
- Payment considerations
- Signature or verbal attestation by the patient
- Prep charts as usual
- Issue appointment reminders to each patient
- Ensure telehealth consent is on file
- While HIPAA guidelines have been "relaxed" during the pandemic, the provider should make every effort to ensure that the telehealth encounter is conducted in a secure area to maintain patient privacy.
- Rendering providers should keep the telehealth interface open and ready for the patient to join the session.
- Upon entering the telehealth "exam room," the provider should consider reminding the patient of the following:
- During this telehealth encounter medical care may be impacted by communication and therefore, the patient is encouraged to be as transparent and blunt about their concerns and complaints as possible.
- Remind the patient that while the provider is taking precautions to ensure privacy as required by HIPAA, the patient's surroundings also pose risks of a HIPAA breach for which the provider/organization cannot be responsible.
- Inform the patient that active treatment and care is being provided during the encounter for their presenting problem, but further workup, testing, treatment, or aftercare is the responsibility of the patient. Non-urgent healthcare services at this time may not be a high priority for referral organizations and therefore the patient may have to make an increased effort to ensure treatment plans are followed.
- The provider should document the encounter as they would a normal, in-person office visit.
- History, to include CC, HPI, ROS, and PFSH should be included as these are all subjective, obtainable through the online interview process with the patient.
- Exams will be limited, but providers are encouraged to consider what is appropriate and medically indicated. Keep in mind that not every patient requires an 8-point organ system exam. Most telehealth patients will support E/M services represented by codes 99212, 99213, or 99214 and therefore the ONLY exam elements required per 1995 documentation guidelines are:
- 99212 - 1 organ system (this could merely be a general statement of the patient's appearance)
- 99213 - 2 organ systems
- 99214 - 2 organ systems with the affected organ system including 3-4 findings. This level of exam may prove difficult in the telehealth setting
- Assessment and plan, which includes the provider's clinical assessment of the complexity of the patient's condition, and a plan of treatment must be included and would not be compromised by the telehealth setting. If the assessment may be limited based on the need for additional workup, this should be noted in the documentation.
- GQ: Asynchronous telehealth service.
- 95: Synchronous telemedicine service rendered via real-time interactive audio and video telecommunications system.
- GT: Critical Access Hospital (CAH) distant site providers billing under CAH Optional Method II*. This goes on an institutional claim and pays 80% of the professional fee schedule rate.
- G0 (zero): Used to identify telehealth services furnished for purposes of diagnosis, evaluation, or treatment of symptoms of an acute stroke (see below).
- GY: Notice of Liability Not Issued, Not Required Under Payer Policy. Used to report that an Advanced Beneficiary Notice (ABN) was not issued because item or service is statutorily excluded or does not meet definition of any Medicare benefit.
References/Resources
About NAMAS
NAMAS is setting the standards in medical auditing & education
The NAMAS team and faculty work hard to bring you membership resources, products, tools, and training that is not only timely and specific to medical auditing and compliance, but also that is specific to the needs of medical practices today. NAMAS staff are industry recognized experts who provide audits and consulting services to active clients which gives NAMAS the cutting edge to provide relevant training.



 Quick, Current, Complete - www.findacode.com
Quick, Current, Complete - www.findacode.com