by Aimee L. Wilcox, CPMA, CCS-P, CST, MA, MT
Apr 19th, 2022
Identifying, treating, and monitoring chronic health conditions is key to reducing a beneficiary's overall risk score. The goal is to help beneficiaries improve upon their health and reduce risk of hospitalization, morbidity, and death. CMS collects and monitors data from claims about the chronic conditions their beneficiaries suffer from. This data is collected on all beneficiaries and compared between traditional Medicare and Medicare Advantage, in an effort to improve quality of care and reduce care costs.
Risk adjustment is the process of estimating predicted health costs for beneficiaries, and how that will impact the reimbursements to healthcare organizations that manage their health plans. Beneficiary health data is gathered throughout the year, reported with ICD-10-CM diagnosis codes, and classified into hierarchical condition categories (HCCs), which carry an assigned risk factor score. The beneficiary's overall risk factor score is linked to a dollar amount that is paid to the healthcare organization managing their health insurance plan for the year.
There are two main models of HCC risk adjustment
- Centers for Medicare and Medicaid Services (CMS) uses the CMS-HCC risk adjustment model, otherwise known as Medicare Part C or Medicare Advantage. This model covers patients enrolled in Medicare.
- The Department of Health and Human Services (HHS) uses the HHS-HCC risk adjustment model. This model covers patients of all ages enrolled in a risk adjustment plan with a commercial payer.
The most important process of risk adjustment reporting is the correct identification of any chronic conditions the beneficiary suffers from, and ensuring they have been properly evaluated, monitored, and treated to reduce the risk of exacerbation, hospitalization, or death.
CMS published a 2018 Chronic Conditions Chart, which contains a significant amount of data related to the number of chronic conditions beneficiaries of the different plans have and the costs associated with each. The following chart (Figure 1) identifies 21 chronic conditions in order of prevalence among Medicare Fee-For-Service (FFS) beneficiaries. Hypertension tops the chart at a whopping 57% of Medicare FFS beneficiaries diagnosed with this condition, with some pretty significant chronic conditions (e.g., cancer, stroke, drug abuse) accounting for less than 10% each.
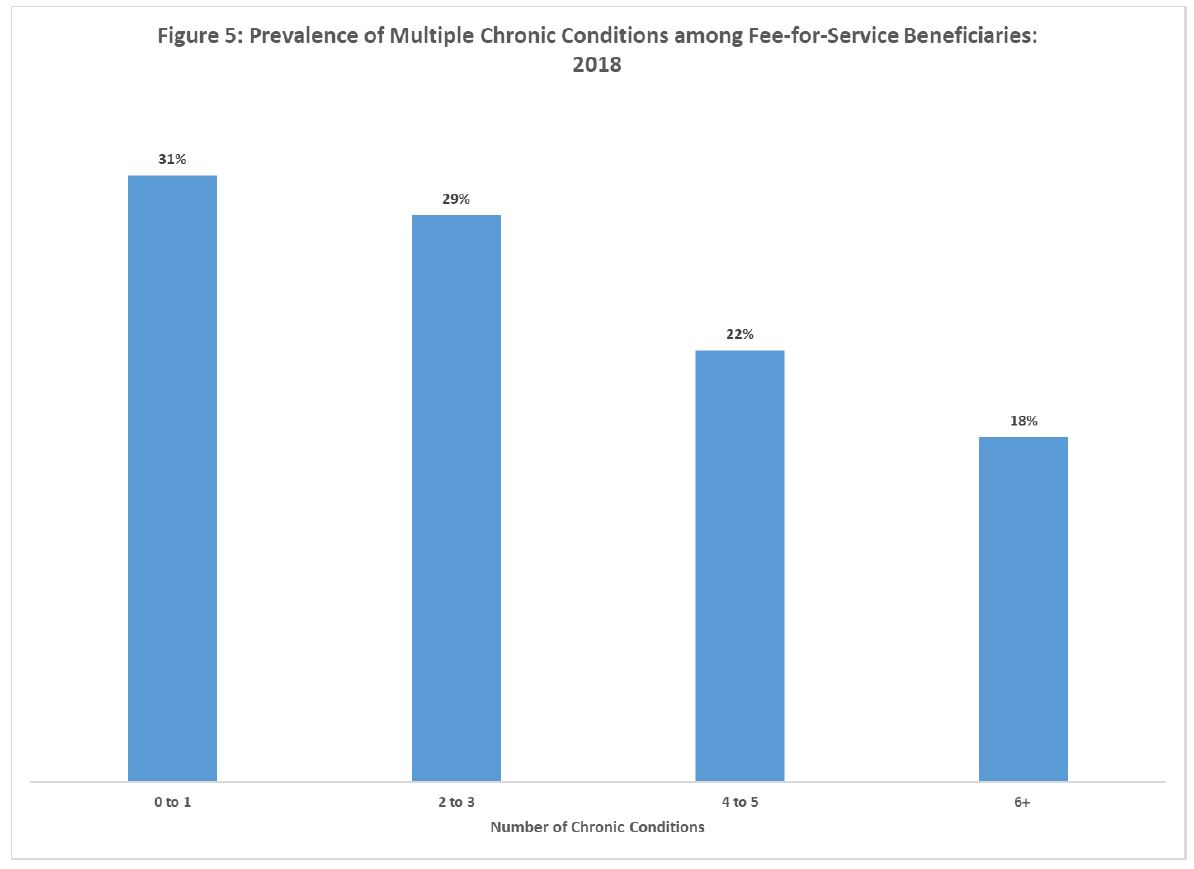
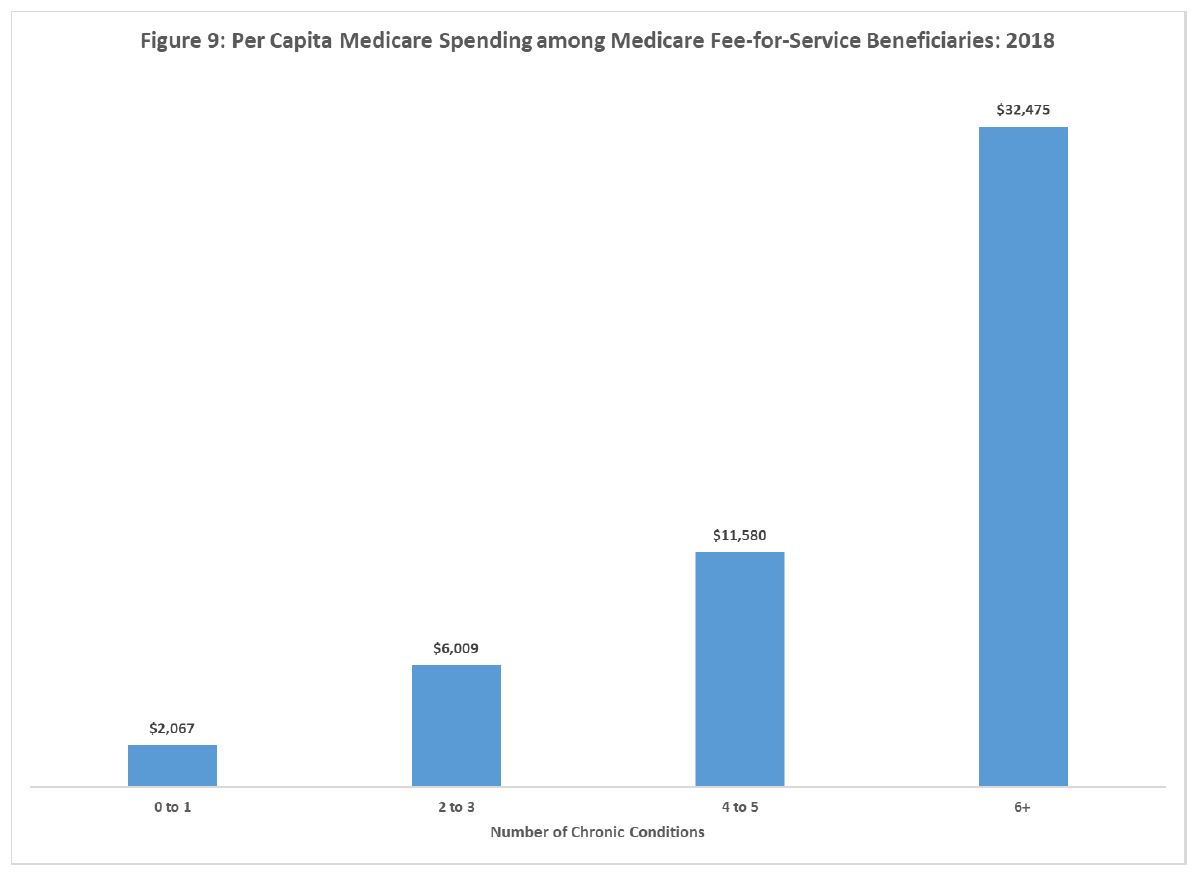
Interestingly, the next two graphs (Figure 5 and Figure 9) show that among Medicare FFS beneficiaries, 31% have 0-1 qualifying chronic conditions with a per capita cost of $2,067, which is tripled with the addition of a third chronic condition and a whopping per capita cost of $32,475 for beneficiaries with six or more chronic conditions.
While higher risk scores result in higher funding to care for healthcare costs, the end goal is to improve health scores (meaning reduce them) and healthcare costs. What are payers doing today to ensure better patient care and improved risk scores? This year (2022) saw added codes to the Care Management Services section of the CPT codes, and revisions to the code descriptions that allow providers to implement a program that is directed, specifically towards patients with chronic conditions who would like assistance in improving them, reducing hospitalizations, and possibly lengthening lifespans. Take the time to review policies that support proactively working towards a lower overall risk score and better health outcomes.
As demonstrated in the above CMS graphs, in 2018, more than two-thirds of Medicare FFS beneficiaries were noted to be living with two more chronic health conditions. As it pertains to changes with risk adjustment, a few significant questions come to the forefront regarding the current health situation:
- Will COVID-19 have an impact on the number of chronic conditions that risk adjustment plan beneficiaries suffer from moving forward?
- How effective is the Medicare Advantage program at controlling the number of treatable chronic conditions as compared with Medicare FFS?
- How is documentation from the public health emergency (PHE) related to the COVID-19 pandemic being tracked and reported for future risk adjustment statistics
We need to push forward in an effort to identify and document chronic conditions that impact the funding needed to ensure proper care of these beneficiaries. One way to accomplish that is to ensure that accurate and effective tools and resources are available for coding and reporting chronic conditions. Coding tools, like HCCCoder, help simplify the process of accurate ICD-10-CM code assignment and quick access to the ICD-10-CM coding guidelines. Take a moment to review the resources available through HCCCoder.
References/Resources
About Aimee L. Wilcox, CPMA, CCS-P, CST, MA, MT
 Aimee L. Wilcox is a medical coding, billing, and auditing consultant, author, and educator with more than 30 years of clinical and administrative experience in healthcare, coding, billing, and auditing. Medicine, including coding and billing, is a constantly changing field full of challenges and learning and she loves both. Aimee believes there are talented medical professionals who, with proper training and excellent information, can continue to practice the art of healing while feeling secure in their billing and reimbursement for such care.
Aimee L. Wilcox is a medical coding, billing, and auditing consultant, author, and educator with more than 30 years of clinical and administrative experience in healthcare, coding, billing, and auditing. Medicine, including coding and billing, is a constantly changing field full of challenges and learning and she loves both. Aimee believes there are talented medical professionals who, with proper training and excellent information, can continue to practice the art of healing while feeling secure in their billing and reimbursement for such care.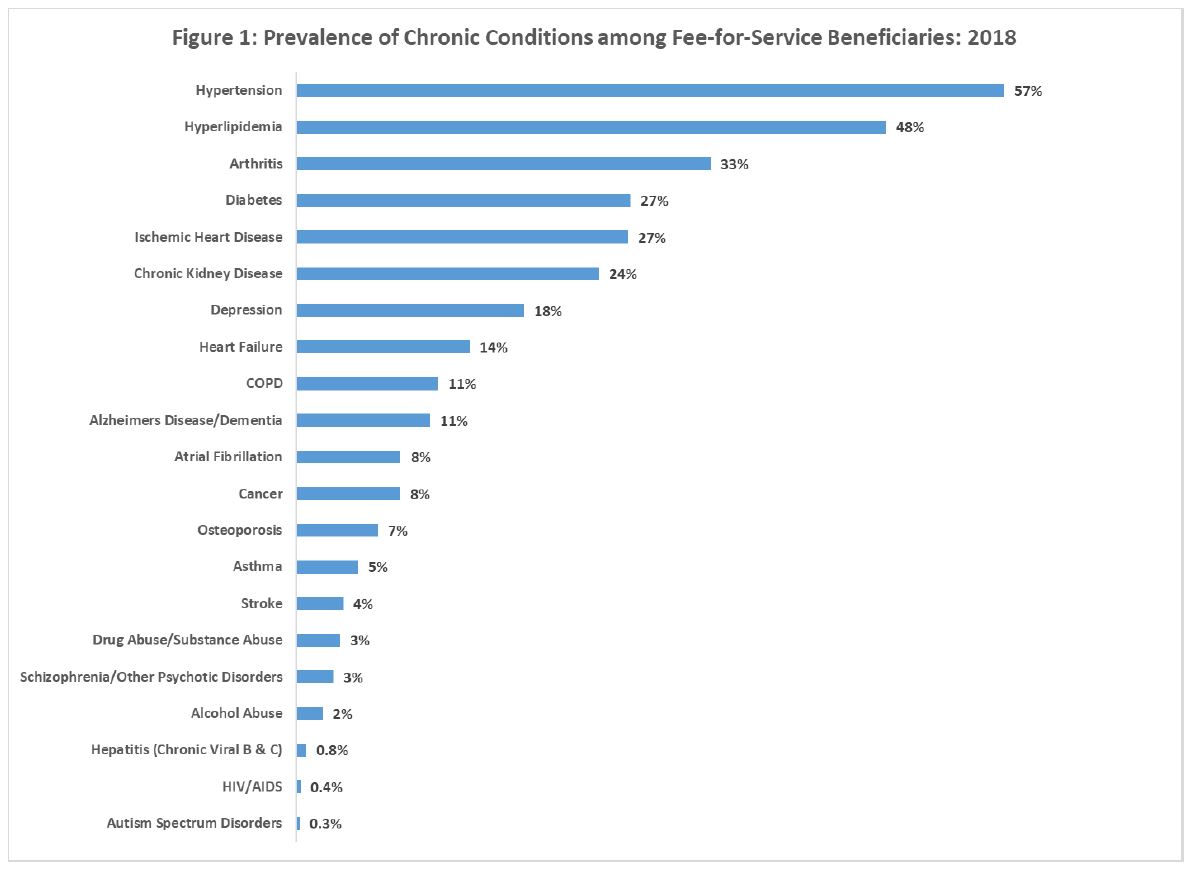

 Quick, Current, Complete - www.findacode.com
Quick, Current, Complete - www.findacode.com